1.
and reproductive health knowledge among children and adolescents is a key component to a healthy life. In Mexico, a country plagued with a teen pregnancy epidemic, sexuality education in the public-school system begins in 4th grade. Our study aims were to characterize the sexual and reproductive health knowledge of middle school students from Oaxaca, and its association with belonging to an indigenous group, gender, sources of sexual and reproductive health information, and parents' level of schooling.
Methods: Cross-sectional study. Students responded to a multiple-choice paper and pencil self-administered survey on sexual and reproductive health knowledge. Our sample included 245 middle-school students (51.4% were female) enrolled in rural school's 7 th , 8 th , and 9 th grade. Survey contents were based on the Ministry of Education textbooks.
Results: Failing scores in individual sections and diagrams were associated with gender and self-identifying as belonging to an indigenous group. Students obtained higher scores in the knowledge-based technical sections vs diagrams. n 2018, Mexico hosted over 22 million adolescents [1] with a fertility rate of 70.6. [2] In 2014, the latter was calculated at 77, representing live births and no record of pregnancies ending in abortion. [3]The country's teen pregnancy epidemic (highest among member countries of the Organization for Economic Cooperation and Development) has not yet fully comprehended and addressed by the government. [4] Oaxaca, a state neighboring Central America, is one of the poorest regions, with a population of 3, 976, 297 [5], of which 65.7% belong to over ten indigenous groups [6] and protestant religions. [7] In a 2015 census, they reported over 800,000 adolescents (10-19 years) and in 2018, 12,127 births were registered to women aged 15-19. [8] Approximately 70% of students in Latin America (LA) do not have access to comprehensive sexual education. A study in five LA countries showed that increasing sexual and reproductive health (SRH) literacy can prevent multiple pregnancies as high school dropouts tend to perpetuate the vicious cycle of teen mothers. The chances of experiencing teen pregnancy increased to 53% among adolescents who had no knowledge of their ovulatory cycle and had never used any form of contraception. [9] Unintended pregnancy leads to a gender-inequity gap that widens and perpetuates the intergenerational poverty cycle. [10] According to UNESCO, "early and unintended pregnancy prevention is one piece of a bigger puzzle", where an effective response from the education sector is needed so adolescents can access quality sexuality education. [11] This is an exploratory, cross-sectional study aimed at documenting adolescent's knowledge on SRH and its correlates with sample characteristics, to better understand the context in which students' from a disadvantaged rural population access information about human sexuality, sexual anatomy, and physiology; reproduction; contraception; as well as correct condom and contraceptive use. We aimed to determine an association between failing scores of enrolled students in knowledge-based and diagrams of the male and female reproductive systems. Assess if their reported sources of information regarding SRH, i.e., parents, teachers, health care centers and the internet, affect their scores.
2. II.
3. Methods
The research team traveled to Oaxaca to meet with the Ministry of Education and school district municipal representatives to explain the study, request authorization to survey middle school students (grades 7 th -9 th , 12-14 years) regarding unmet SRH information needs. The ad-hoc study questionnaire was drafted in collaboration with local partners and adapted to the local context. We carried out a pilot phase among students attending the same school years. As students were underage, we convened a meeting with parents and school principals to obtain informed consent, given the sensitive nature of some questions. We began data collection with partners from Oaxaca State University. All 245 students (male and female) enrolled in grades 7 th , 8 th , and 9 th were eligible and invited to participate, the survey content was explained, and consent requested. All students agreed and signed an informed consent form. Our response rate was 100%. We selected 3 public middle schools located in the Tlacolula, Etla, and Centro school districts. We used convenience sampling and selection bias was addressed by selecting similar public schools (State of Oaxaca Human Development Index (HDI): 0.67; San PedroIxtlahuaca HDI: 0.64-0.70; San Juan del Estado HDI: 0.64-0.70; San Sebastián Teitipac HDI: 0.59-0.64), [12] and geographically distant while belonging to the region. Fieldwork started after the study protocol was submitted to UNAM's Internal Review Board and approved: FM-DI-028-2017.
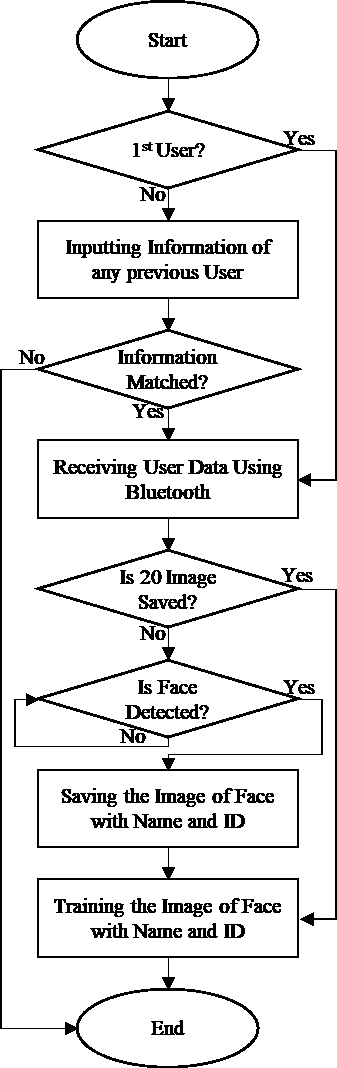
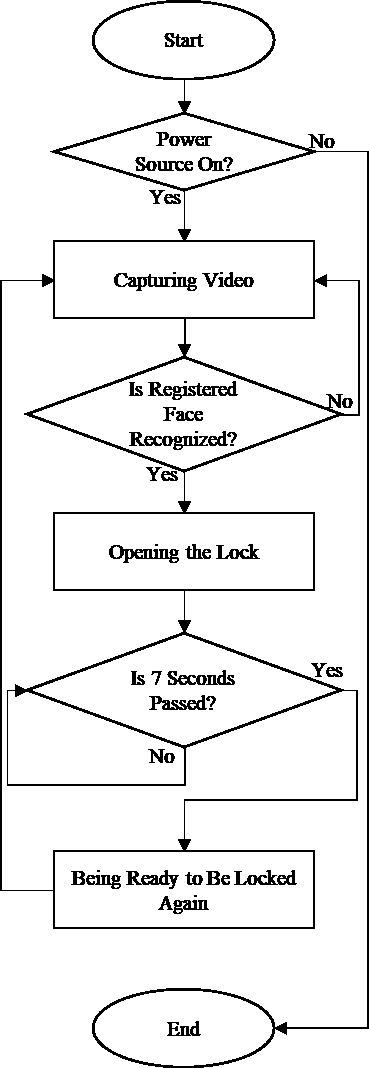
Ours was a cross-sectional study that included a multiple-choice paper and pencil self-administered survey with 9 questions covering demographics, 24 questions divided in 3 sections assessing technical knowledge and 5 diagrams. Every participant received colored diagrams, a response sheet, and a survey booklet. Diagram design followed international guidelines. [13,14] (Appendix A). Section 1: female sexuality (Q#1-7), Section 2: male sexuality (Q#8-12), Section 3: modern contraceptive methods (MCM), sources of SRH information (Q# [13][14][15][16][17][18][19][20][21][22]. Diagrams were subdivided into five categories: a) female reproductive system (FRS), b)male reproductive system (MRS), c) anatomical placement of MCM, d) diagrams associated with MCM, and e) 9 steps for correct male condom placement. Sections and diagrams were scored as follows; a failing score included having <60% of incorrect questions. Each question in every section was scored individually, and we obtained a score for the entire survey (3 sections). For the diagram illustrating correct condom placement, students had to correctly identify all 9 to score it correctly. Students took on average 60 minutes to respond to the survey, and we stood by to respond to questions/queries. Students had a day off to participate and answer the survey in their classroom during routine school hours. Survey questions were based on public textbooks from grades 4th, 5th, and 6th. In Mexico, sexuality education begins in the public-school system in grade school four, according to the Ministry of Public Education SRH guidelines. Our questions were based on textbooks and included the minimal level of information every student needs to cover before graduating and enroll in their current school year (Appendix B). We included information only covered in grade 7 because the recent education reform does not include health sciences in grades 8 and 9 (peak years for teen pregnancy). Analysis included all 245 students. We describe sample characteristics, family structure, belonging to an indigenous group, family structure, parents' level of schooling, and year currently enrolled in students classified as failing in the three individual sections, the entire survey, and the diagrams. Variables were included as frequencies and proportions and we determined their association with failing scores using chi-square tests. The dependent variable was obtaining a failing score in individual sections and a failing score for the entire survey and the diagrams. Sample characteristics and sources of SRH information were considered independent variables. We used logistic regression models and the probability of failing associated with sample characteristics and sources of SRH information. Alpha levels were set at 0.05, we calculated odd ratios and carried out statistical analysis, SPSS v. 25. [15] Diagram 1: Female reproductive system
4. Results
The school distribution for all 245 students was school A; 50.6% (n=124, 48.4 female), school B; 32.2% (n=79, 45.6% female) and school C; 17.1% (n=42, 71.4 % female). We did not find significant differences across schools in total failing scores (p>0.05). All 245 students that were invited to participate responded to the selfadministered survey, with a 100% response rate. 51.4% were women; mean age was 13.06 (SD=1.0, p=0.061).
34.3% were currently enrolled in 7 th , 30.2% in 8 th and 35.5% in 9 th grade. The gender distribution across all years was similar (p>0.05) (Table 1). Only 12.5% (14 women, 15 men) self-identified as belonging to an indigenous group (we did not enquire language spoken at home, last name, the region of origin, nor skin color). [16] 76.8% of mothers and 77.7% of fathers had completed at least 10 years of schooling (above the 7.5 state average). [17] Table 1 Prevalence failing scores per individual sections were FRS (15.9%), MRS (24.9%), knowledge of MCM (30.6%), and failing score for the entire survey was 34.3%. Table 2 describes the failing scores per section, failing scores for the entire survey and associations by sample characteristics. Failing scores for the FRS were associated with gender and belonging to an indigenous group (p<0.05). Failing scores for knowledge of MCM were associated with gender and mother's age (p<0.05). Failing scores for the entire survey were associated with gender and belonging to an indigenous group (p<0.05). All failing scores in individual sections and the entire survey were associated with students' year of enrollment, with a higher proportion of students in grade 7th with failing scores (individual and total scores). Students responses to section B included diagrams displaying the anatomical representation of the female and MRS, the anatomical placement and visual recognition of MCM, and a diagram of correct condom placement. The failing score prevalence for the FRS was 50.2%, for the MRS 44.5%, for anatomical placement of MCM 64.9%, for visual recognition of MCM 24.5% and for the diagram of correct condom placement; 20.4%. Table 3 shows how the schematic representation of the FRS and the diagram for correct condom placement were associated with the school year currently enrolled in (p<0.05). We found an association among students with failing scores in visual recognition of MCM; 92% of those who failed did not report using the internet as a source of SRH information, and 96% of those who failed the section on correct condom use (p=0.004). We found an association between failing scores in the male and FRS diagrams, and approaching their father as a source of SRH information (p<0.05); however, 34 and 36% of students who approached their father failed both the male and reproductive systems. After bivariate analysis (Appendix C) we carried out the multivariate analysis. Table 4 includes sample characteristics (gender, school year, indigenous group, and source of SRH information) and its association with failing scores in knowledge-based sections. The failing scores for the FRS were associated with gender; males had a five-fold risk of failing this section compared to women (OR 5.12 [CI 95% 2.12-12.37]), self-identifying as belonging to an indigenous group had an approximate four-fold risk of failure (OR 4.50 [CI 95% 1.71-11.8]), being enrolled in higher years 8th or 9th was a protective factor (OR 0.26 [CI 95% 0.10-0.69]) and (OR 0.33 [CI 95% 0.12-0.87]) respectively. Gender was associated with failing the section on knowledge of MCM; men had a two-fold risk of failing (OR 2.16 [CI 95% 1.20-3.89]). Students who used the Internet as a source for SRH information displayed a protective factor when answering MRS (OR 0.30 [CI 95% 0.10-0.90]). Being male was associated with failing sections on knowledge of MCM (OR 2.16 [CI 95% 1.20-3.89]) and with year enrolled in; when they reach grade 9 (compared to 8th(OR 0.51 [CI 95% 0.26-0.41]) being in school seems to be less protective (OR 0.20 [CI 95% 0.09-0.41]).
Failing scores for the entire survey were associated with gender and indigenous group; men had a (OR 2.23 [CI 90% 1.21-4.09]) and those self-identified as indigenous (OR 2.11 [CI 90% 0.89-5]). For failing scores in the entire survey, being male was also a risk factor and enrolled in 8 th grade (OR 0.26 [CI 95% 0.13-0.54]) and 9 th (OR 0.23 [CI 95% 0.11-0.48]) was protective (Table 4). Gender was not associated with failing scores in students' recognition of diagrams. When students were asked to identify diagrams of the female and MRS, being in 9th grade (vs 7th) was considered a protective factor for not failing the diagrams of the FRS (OR 0.43 [CI 95% 0.23-0.81]). We found an association between being enrolled in grade 8th and not failing the MRS diagram (OR 0.37 [CI 95% 0.17-0.82]). Students (male and female) who asked their fathers about SRH information compared to those who did not, had an almost two-fold risk of failing the section on the FRS (OR 1.90 [CI 95% 1.05-3.43]) and the MRS (OR 2.48 [CI 95% 1.24-4.96]). Failing scores on anatomical placement of MCM were significantly associated with father's level of schooling; those with completed high school (compared with those with <high school) yielded an (OR 0.49 [CI 95% 0.25-0.95]). Students self-identifying as indigenous had a two-fold risk of failing the visual recognition of MCM (OR 2.38 [CI 95% 1.05-5.42]) and using the internet as a source of reference for this section was a protective factor (OR 0.33 [CI 95% 0.12-0.89]). Lastly, failing scores for correct condom placement were associated with the use of the internet as a source of SRH information as a protective factor(OR 0.18 [CI 95% 0.04-0.81])(Table 5). IV.
5. Discussion
Our exploratory study describes SRH knowledge among students currently enrolled in 7th, 8th, and 9th grade in a rural public middle school in Oaxaca. We found an association between grade of enrollment and knowledge of male and FRS; school appears to be a protective factor as there is a slight difference between grades 8 and 9, however, knowledge of MCM decreases by grade 9 when they are most in need of information as the median age for adolescent's sexual debut is 15, our participants have scant knowledge of MCM, [18] and Oaxaca is the third state with the highest rate of teen pregnancy.[19] In Mexico, adolescents receive sex education from public schools and most sexuality education topics are covered by middle school. [20,21] While the content would need to be consistent with the grade level, our results show otherwise. Basic knowledge of male and FRS is taught in middle school and reviewed in grade 7 th together with MCM. So as not to create detrimental information gaps, students would need to continue receiving information on MCM during grades 8 and 9 to comply with UNESCO's 2009 guidelines on comprehensive sexuality education curricula. [22] Adolescents face significant challenges when accessing and learning about consistent contraceptive use. We showed ethnic inequities among students selfidentifying as indigenous vs those who do not. In our study, 12.5% of students who self-identified as indigenous (in Oaxaca 65.7% belong to one) had a twofold risk (2.38) of failing the visual recognition of MCM and a four-fold risk of failing the FRS. In 2014 women who spoke an indigenous language reported a higher uptake of MCM in their first sexual encounter compared with data from 2009 (4.9% vs 11.8%). The reasons why indigenous women do not access MCM is primarily due to a lack of knowledge of where to obtain them and not knowing how to use them. [23] In our question on correct condom use, only 20% failed, 24.5% failed the visual recognition of MCM and 64.9% failed the anatomical placement of MCM. If students are unable to correctly identify the anatomical site of MCM this will become their strongest barrier to use, together with the fact that they are unable to identify them. The latter is consistent with data from surveys where 84.5% of women report using condoms in the first sexual encounter. [23] As per our results, this may due to their lack of information on other MCM with higher effectiveness rates; Mexican adolescents continue favoring condoms over other effective methods as part of their sexual debut. A third of adolescents (28.6%) who chose not to use a contraceptive method during their first sexual encounter reported "not knowing where to get them or how to use them" [23], which is consistent with the 24.5% of our participants being unable to visually identify MCM. Gender (male) was associated with failing scores in all the knowledge-based sections; FRS and MCM. In contrast, male (50.9%) and female (49.1%) students had similar failing scores in diagrams; both were unable to identify anatomical placement of MCM, visual recognition of MCM showed similar failing scores (50% vs 50%). In traditional societies, the responsibility of contraception is often placed in the hands of women, we may hypothesize that our male participants are failing the knowledge questions because they are replicating the standard where they do not feel it is up to them to prevent a pregnancy; thus are not fully engaged in SRH programs and it appears as if condoms are their only viable alternative. A recent ethnographic study done in rural communities with the highest teen pregnancy rates reports girls also expect their boyfriend/partner will take care of them (i.e., use a MCM) in their first sexual encounter. [24] We also explored the sources of SRH information reported by students. In our multivariate analysis, we did not find an association between failing any section (knowledge and diagrams) and approaching teachers, friends/ boyfriend/girlfriend, and not approaching anyone. We found an association between internet use and knowledge of the MRS, visual recognition of MCM, and correct condom use. Our prevalence of internet use (17%) was high considering that in 2018, 5.3% of rural households in Oaxaca reported having internet access [25]; therefore. we estimate that students may be accessing SRH on their mobile phones. [26] Evidence suggests mobile phones are useful to reach vulnerable populations and have the potential to generate changes in knowledge and behavior. [26,27] We need to implement a strategic approach whereby adolescents access SRH education and services via m Health-use of mobile phones to improve health behaviors and services-a technical area that has witnessed an increased interest and promise in high and middleincome countries. [26] Of all internet users in Oaxaca, 23.6% access it in school and 24% in free public spaces. [25] Despite limited internet access among this population, the internet was considered an adequate learning tool in our study as it provided sufficient knowledge, and its use improved students' scores. It was the most reliable source of SRH information regarding knowledge of the MRS and visual recognition of MCM.
Parents have a unique opportunity to transmit knowledge and information about potential sexual risks and instill confidence and safety around adolescents' sexual choices. [28] Strategies parents adopt regarding SRH have repercussions on adolescent's sexual behavior; however, most parent-adolescent SRH communication research comes from high-income countries, and there is a dearth of information in low-and middle-income countries (LMIC). [29] Adolescents from LMIC, living in rural areas, continue to face social and health challenges. [30] However, in our study, male and female students who approached their father (52.6% had primary school or no schooling) as a source of SRH information, were associated with 1.9 greater risk of failing. In a traditional society such as Oaxaca, what students learn about SRH is taught by their father and not their mother. [31] If parents are sensitized about the risks that adolescence involves, will be easier to promote sexuality education, prevention of sexually transmitted infections and unintended pregnancy through more effective parent-adolescent communication strategies, and evidence-based SRH information. [32] Parents need to know that in Mexico, 23% of adolescents begin their sexual life between 12-19 years; of these, 15% of men and 33% of women did not use any MCM in their first sexual encounter. Thus, according to these data, approximately 340,000 births occur per year in women under 19. [33] One of the biggest challenges SRH education has is the way it is taught to children and adolescents. In our study, the biggest hurdle was students' difficulty to correctly identify diagrams of the male and FRS, anatomical placement of MCM, and correct identification of MCM. To promote the inclusion of students from rural areas, we need to implement innovative and effective online teaching methods (i.e., WhatsApp) while acknowledging internet access is poor. A study examined the impact of audio-visual media in SRH knowledge among 153 middle-school students. Findings showed that audiovisual media significantly improves SRH knowledge among adolescents. [34] If our study participants displayed more difficulty in sections involving diagrams (vs the knowledge-based questions), perhaps we must center our efforts on learning tools with graphic and brief content that have the potential to "remain in the minds of those who simply glance at them". [35] In the context of the SARS-CoV-2 pandemic, the government estimates that between 2020-2021 there will be a 20% increase in teen pregnancies equivalent to 21,575 pregnancies associated with an unmet contraceptive need. [36] If we take into account that: a) schools closed as of March 23, 2020 and education is currently offered via television; b) schools in rural settings traditionally have limited resources, lack adequate infrastructure including trained teachers in charge of providing evidence-based SRH information; c) there has been an increase in school desertion; d) the absence of the lay state complicates the lack of available information parents of adolescents have regarding SRH topics; e) Mexico hosts a teen pregnancy epidemic; f) our study participants had a high percentage of failing scores when asked about SRH topics they had covered during primary school. The latter points towards a pressing need to promote SRH education at all levels of middle school to help reduce adolescent pregnancy.
V.
6. Conclusion
The internet must become an alternative learning medium on SRH topics and part of traditional teaching especially because the information our participants receive from their parents is inadequate and was associated with the risk of obtaining failing scores. SRH must be taught as a continuum and not only in grade 7th because school decreases as a protective factor as the year of enrollment increases. Our data was collected before the SARS-CoV-2 pandemic. As online education becomes an integral part of the New Normal, Oaxaca's government will need to expand/ strengthen internet coverage for students to continue learning the context-specific SRH curricula that will allow them to flourish.
7. Study limitations:
We only surveyed three public middle schools, and while we got a 100% response rate, we would benefit from sampling schools from other regions. Our methodology does not allow for causal inferences about the associations found, and we were unable to follow-up our participants to enquire if after their participation, they had sought other sources of SRH information. Students belonging to an indigenous group were at a disadvantage; a translation of the survey into their language would reflect more accurately their level of knowledge and eliminate the bias of responding in Spanish.
8. List of abbreviations
LA-Latin America SRH-Sexual and reproductive health HDI-Human Development Index MCM-Modern Contraceptive Methods FRS-Female reproductive system MRS-Male reproductive system LMIC-Low-and middle-income countries
9. Declarations
Ethics approval and consent to participate: Faculty of Medicine (IRB #: FM-DI-028-2017).
10. Availability of data and materials:
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
| Women | Men | p-value | Total | |
| 126 (51.4) | 119 (48.6) | 0.654 | 245 | |
| Age(?? ?) | 12.9 (0.9) | 13.18 (1.1) | 0.061 | 13.06 (SD=1.0) |
| n (%) | n (%) | ?² | n (%) | |
| School year currently enrolled in (grade) | ||||
| 7th | 48 (38.1) | 36 (30.3) | 0.206 | 84 (34.3) |
| 8th | 32 (25.4) | 42 (35.3) | 74 (30.2) | |
| 9th | 46 (36.5) | 41 (34.5) | 87 (35.5) | |
| Belongs to indigenous group (self-report) | ||||
| No | 106 (88.3) | 98 (86.7) | 0.710 | 204 (87.5) |
| Yes | 14 (11.7) | 15 (13.3) | 29 (12.5) | |
| Family structure (lives with) | ||||
| Both parents | 87 (69) | 86 (72.3) | 0.824 | 173 (70.6) |
| Mother | 34 (27) | 28 (23.5) | 62 (25.3) | |
| Father, grandfather, uncle | 5 (4) | 5 (4.2) | 10 (4.1) | |
| Mother's level of schooling | ||||
| Up to high school | 60 (54.1) | 41 (42.7) | 0.190 | 101(48.8) |
| High school | 30 (27) | 28 (29.2) | 58 (28.0) | |
| High school+ | 21 (18.9) | 27 (28.1) | 48 (23.2) | |
| Father's level of schooling | ||||
| Up to high school | 48 (52.2) | 44 (53) | 0.119 | 92 (52.6) |
| High school | 28 (30.4) | 16 (19.3) | 44 (25.1) | |
| High school+ | 16 (17.4) | 23 (27.7) | 39 (22.3) | |
| Mother's age range (yrs) | ||||
| <30 | 11 (8.9) | 16 (14.4) | 0.287 | 27 (11.5) |
| 30 -40 | 66 (53.2) | 61(55) | 127 (50.0) | |
| 40+ | 47(37.9) | 34 (30.6) | 81 (34.5) | |
| Father's age range (yrs) | ||||
| <30 | 4(3.5) | 4 (3.8) | 0.703 | 8 (3.7) |
| 30 -40 | 45(39.8) | 47 (45.2) | 92 (42.4) | |
| 40+ | 64(56.6) | 53 (51) | 117 (53.9) | |
| *?² test, 95% |
| Failing scores in individual sections | ||||||||
| Female reproductive | Male reproductive | Knowledge of | Failing scores for entire | |||||
| system | system | contraceptive methods | survey | |||||
| Sample characteristics | n=39 (15.9%) | n=61 (24.9%) | n=75 (30.6%) | n=84 (34.3%) | ||||
| n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | |
| School year currently enrolled | ||||||||
| in (grade) | ||||||||
| 7 th | 23(59) | 0.002 | 30(49.2) | 0.018 | 38(50.7) | <0.001 | 46(54.8) | <0.001 |
| 8 th | 8(20.5) | 15(24.6) | 24(32) | 20(23.8) | ||||
| 9 th | 8(20.5) | 16(26.2) | 13(17.3) | 18(21.4) | ||||
| Gender | ||||||||
| Women | 10(25.6) | <0.001 | 30(49.2) | 0.685 | 30(40) | 0.017 | 35(41.7) | 0.027 |
| Men | 29(74.4) | 31(50.8) | 45(60) | 49(58.3) | ||||
| Belongs to indigenous group | ||||||||
| (self-report) | ||||||||
| No | 25(69.4) | <0.001 | 47(81) | 0.083 | 61(83.6) | 0.212 | 66(81.5) | 0.040 |
| Yes | 11(30.6) | 11(19) | 12(16.4) | 15(18.5) | ||||
| Mother's age range (yrs) | ||||||||
| <30 | 10(25.6) | 0.091 | 10(16.9) | 0.301 | 13(18.6) | 0.037 | 13(16.5) | 0.170 |
| 30 -40 | 14(38.9) | 29(49.2) | 39(55.7) | 43(54.4) | ||||
| 40+ | 15(41.7) | 20(33.9) | 18(25.7) | 23(29.1) | ||||
| Source of SRH information | ||||||||
| The Internet | ||||||||
| No | 37(94.1) | 0.023 | 57(93.4) | 0.007 | 66(88) | 0.107 | 77(91.7) | 0.005 |
| Yes | 2(5.1) | 4(6.6) | 9(12) | 9(12) | ||||
| Teacher | ||||||||
| No | 35(89.7) | 0.123 | 54(88.5) | 0.078 | 67(89.3) | 0.025 | 76(90.5) | 0.006 |
| Yes | 4(10.3) | 7(11.5) | 8(10.7) | 8(9.5) | ||||
| Father | ||||||||
| No | 24(61.5) | 0.093 | 39(63.9) | 0.082 | 55(73.3) | 0.853 | 54(64.3) | 0.036 |
| Yes | 15(38.5) | 22(36.1) | 20(26.7) | 30(35.7) | ||||
| Failing scores for diagrams | ||||
| Female | Male | Anatomical | Visual recognition | Schematic diagram |
| reproductive | reproductive | placement of | of contraceptive | of correct condom |
| system schematic | system | contraceptive | methods | placement (9 |
| diagram | schematic | methods | n=60 (24.5%) | steps) |
| n=123 (50.2%) | diagram | n=159 (64.9%) | n=50 (20.4%) | |
| n=109 (44.5%) |
| Failing scores | ||||||||
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
| Female reproductive | Male reproductive | Knowledge of | Entire survey | |||||
| system | system | contraceptive methods | ||||||
| Sample characteristics | OR | CI 95% | OR | CI 95% | OR | CI 95% | OR | CI 95% |
| Gender | ||||||||
| Women | 1 | 1 | 1 | |||||
| Men | 5.12** * | (2.12 -12.37) | - | - | 2.42*** | (1.33 -4.41) | 2.23*** | 1.21-4.09 |
| School year currently | ||||||||
| enrolled in (grade) | ||||||||
| 7th | 1 | 1 | 1 | 1 | ||||
| 8th | 0.26** * | (0.10 -0.69) | 0.49* | (0.23 -1.01) | 0.50** | (0.25 -0.98) | 0.26*** | (0.13 -0.54) |
| 9th | 0.33** | (0.12 -0.87) | 0.50* | (0.24 -1.03) | 0.20*** | (0.09 -0.42) | 0.23*** | (0.11 -0.48) |
| Belongs to an indigenous | ||||||||
| group (by self-report) | ||||||||
| No | 1 | 1 | ||||||
| Model 1 Female reproductive system schematic diagram | Model 2 Male reproductive system schematic diagram | Model 3 Anatomical placement of contraceptive methods | Model 4 Visual recognition of CM | Model 5 Schematic diagram of correct condom placement (9 steps) | ||||||
| Failing scores: | OR | CI 95% | OR | CI 95% | OR | CI 95% | OR | CI 95% | OR | CI 95% |
| School year currently | ||||||||||
| enrolled in (grade) | ||||||||||
| 7th | 1 | 1 | 1 | |||||||
| 8th | 0.70 | (0.36 -1.33) | 0.37** | (0.17 -0.82) | - | - | - | - | 1.19 | (0.56 -2.52) |
| 9th | 0.39** * | (0.21 -0.74) | 0.67 | (0.31 -1.48) | - | - | - | - | 0.34** | (0.13 -0.85) |
| Belongs to an | ||||||||||
| indigenous group (by | ||||||||||
| self-report) | ||||||||||
| No | 1 | |||||||||
| Yes | - | - | - | - | - | - | 2.38** | (1.05 -5.42) | - | - |
| Father's level of | ||||||||||
| schooling | ||||||||||
| 1 | ||||||||||
| High school | - | - | - | - | 0.49* * | (0.25 -0.95) | - | - | - | - |
| High school + | - | - | - | - | 0.64 | (0.31 -1.32) | - | - | - | - |
| Source of SRH | ||||||||||
| information: | ||||||||||
| Mother | ||||||||||
| No | 1 | |||||||||
| Yes | 0.35** * | (0.18 -0.69) | ||||||||
| Father | ||||||||||
| No | 1 | 1 | ||||||||
| Yes | 2.08** | (1.14 -3.79) | 2.48** | (1.24 -4.96) | - | - | - | - | - | - |
| The Internet | ||||||||||
| Failing scores in individual sections | Failing scores for entire survey | |||||||
| Failing scores: | Female reproductive system | system Male reproductive | Knowledge of methods contraceptive | Failing scores for entire survey | ||||
| OR | CI 95% | OR | CI 95% | OR | CI 95% | OR | CI 95% | |
| Gender | ||||||||
| Men | 3.74*** | (1.73 -8.07) | 1.13 | (0.63 -2.01) | 1.95** | (1.12 -3.38) | 1.82** | (1.07 -3.10) |
| School year currently | ||||||||
| enrolled in (grade) | ||||||||
| 8th | 0.32** | (0.13 -0.77) | 0.46** | (0.22 -0.94) | 0.58 | (0.30 -1.11) | 0.31*** | (0.16 -0.60) |
| 9th | 0.27*** | (0.11 -0.64) | 0.41** | (0.20 -0.82) | 0.21*** | (0.10 -0.44) | 0.22*** | (0.11 -0.42) |
| Belongs to indigenous | ||||||||
| group (by self-report) | ||||||||
| Yes | 4.38*** | (1.85 -10.33) | 2.04* | (0.90 -4.62) | 1.65 | (0.75 -3.67) | 2.24** | (1.02 -4.91) |
| Family structure (lives | ||||||||
| with) | ||||||||
| Mother | 1.42 | (0.66 -3.04) | 1.08 | (0.56 -2.11) | 0.73 | (0.38 -1.39) | 0.58* | (0.30 -1.10) |
| Father/other | 1.48 | (0.30 -7.38) | 1.34 | (0.33 -5.40) | 0.90 | (0.22 -3.59) | 0.71 | (0.18 -2.85) |
| Mother's level of schooling | ||||||||
| Grade school | 1.39 | (0.60 -3.18) | 0.91 | (0.44 -1.89) | 0.98 | (0.48 -1.99) | 1.00 | (0.50 -2.00) |
| Grade school + | 0.76 | (0.28 -2.08) | 0.37** | (0.14 -0.97) | 0.88 | (0.41 -1.89) | 0.69 | (0.32 -1.49) |
| Father's level of schooling | ||||||||
| Grade school | 0.81 | (0.29 -2.26) | 0.83 | (0.36 -1.94) | 1.12 | (0.53 -2.38) | 0.83 | (0.38 -1.80) |
| Grade school+ | 1.12 | (0.42 -3.01) | 0.73 | (0.30 -1.81) | 0.51 | (0.21 -1.24) | 0.77 | (0.34 -1.76) |
| Mother's age range (yrs) | ||||||||
| 30 -40 | 0.35** | (0.13 -0.99) | 0.50 | (0.21 -1.22) | 0.48* | (0.21 -1.11) | 0.55 | (0.24 -1.28) |
| > 40 | 0.65 | (0.23 -1.81) | 0.56 | (0.27 -1.28) | 0.31** | (0.12 -0.77) | 0.43* | (0.17 -1.05) |
| Father's age range (yrs) | ||||||||
| 30 -40 | 1.15 | (0.13 -10.15) | 1.00 | (0.19 -5.30) | 0.93 | (0.21 -4.15) | 0.98 | (0.22 -4.35) |
| >40 | 1.27 | (0.15 -10.98) | 0.94 | (0.18 -4.94) | 0.63 | (0.14 -2.78) | 0.77 | (0.17 -3.40) |
| *** p<0.01, ** p<0.05, * p<0.1 | ||||||||
| 8th | 0.80 | (0.43 -1.50) | 0.94 | (0.50 -1.76) | 0.62 | (0.32 -1.21) | 0.93 | (0.46 -1.86) | 1.27 | (0.62 -2.59) |
| 9th | 0.42** * | (0.22 -0.77) | 0.64 | (0.35 -1.18) | 0.65 | (0.34 -1.24) | 0.56 | (0.27 -1.16) | 0.37** | (0.16 -0.87) |
| Belongs to | ||||||||||
| indigenous group | ||||||||||
| (by self-report) | ||||||||||
| Yes | 1.47 | (0.67 -3.24) | 1.59 | (0.73 -3.48) | 0.97 | (0.43 -2.20) | 2.36* * | (1.05 -5.29) | 1.97 | (0.83 -4.66) |
| Family structure | ||||||||||
| (lives with) | ||||||||||
| Mother | 0.73 | (0.41 -1.31) | 0.49 ** | (0.27 -0.91) | 0.66 | (0.36 -1.20) | 0.52* | (0.24 -1.10) | 0.60 | (0.27 -1.33) |
| Father/other | 2.20 | (0.55 -8.80) | 0.69 | (0.19 -2.53) | 0.72 | (0.19 -2.65) | 1.15 | (0.29 -4.63) | 1.52 | (0.38 -6.17) |
| Mother's level of | ||||||||||
| schooling | ||||||||||
| Grade school | 0.84 | (0.44 -1.60) | 1.01 | (0.53 -1.94) | 0.49 ** | (0.25 -0.95) | 0.68 | (0.31 -1.49) | 0.79 | (0.36 -1.77) |
| Grade school+ | 1.10 | (0.56 -2.20) | 0.82 | (0.41 -1.64) | 0.64 | (0.31 -1.32) | 0.76 | (0.33 -1.74) | 0.68 | (0.28 -1.65) |
| Father's level of | ||||||||||
| schooling | ||||||||||
| Grade school | 1.19 | (0.58 -2.45) | 0.45 ** | (0.21 -0.95) | 0.39 ** | (0.18 -0.82) | 0.94 | (0.41 -2.16) | 0.63 | (0.26 -1.54) |
| Grade school + | 0.94 | (0.44 -1.98) | 0.74 | (0.35 -1.57) | 0.63 | (0.28 -1.41) | 0.85 | (0.35 -2.05) | 0.42 | (0.15 -1.19) |
| Mother's age | ||||||||||
| range (yrs) | ||||||||||
| 30 -40 | 0.64 | (0.27 -1.48) | 1.52 | (0.65 -3.58) | 0.62 | (0.24 -1.57) | 0.62 | (0.25 -1.52) | 0.44* | (0.18 -1.11) |
| 40+ | 0.61 | (0.25 -1.47) | 1.23 | (0.50 -3.02) | 0.60 | (0.23 -1.57) | 0.61 | (0.24 -1.59) | 0.53 | (0.20 -1.39) |
| Father's age | ||||||||||
| range (yrs) | ||||||||||
| 30 -40 | 0.53 | (0.12 -2.33) | 3.00 | (0.58 -15.65) | 1.24 | (0.28 -5.54) | 1.06 | (0.20 -5.61) | 0.89 | (0.17 -4.73) |
| 40+ | 0.68 | (0.15 -2.96) | 2.24 | (0.43 -11.56) | 1.11 | (0.25 -4.89) | 0.94 | (0.18 -4.94) | 0.82 | (0.15 -4.29) |
| *** p<0.01, ** p<0.05, * p<0.1 | ||||||||||
| Failing scores in individual diagrams | ||||||||||
| Failing scores: | Female reproductive system schematic diagram | Male reproductive system schematic diagram | Anatomical placement of contraceptive method | Visual recognition of CM | Schematic diagram of correct condom placement (9 steps) | |||||
| OR | CI 95% | OR | CI 95% | OR | CI 95% | OR | CI 95% | OR | CI 95% | |
| Gender | ||||||||||
| Men | 1.51 | (0.91 -2.49) | 1.00 | (0.61 -1.66) | 1.31 | (0.77 -2.22) | 1.08 | (0.60 -1.93) | 0.88 | (0.47 -1.64) |
| School year | ||||||||||
| currently enrolled | ||||||||||
| in (grade) | ||||||||||
| Friends | ||||||||
| No | 36(92.3) | 0.692 | 59(96.7) | 0.059 | 70(93.3) | 0.332 | 79(94) | 0.183 |
| Yes | 3(7.7) | 2(3.3) | 5(6.7) | 5(6) | ||||
| Health care center | ||||||||
| No | 31(79.5) | 0.303 | 53(86.9) | 0.617 | 69(92) | 0.039 | 74(88.1) | 0.313 |
| Yes | 8(20.5) | 8(13.1) | 6(8) | 6(8) | ||||
| Boyfriend/girlfriend | ||||||||
| No | 30(50) | 0.380 | 61(100) | 0.246 | 75(100) | 0.180 | 83(98.8) | 0.693 |
| Yes | 0(0) | 0(0) | 0(0) | 1(1.2) | ||||
| The Internet | ||||||||
| No | 13(21.7) | 0.023 | 57(93.4) | 0.007 | 66(88) | 0.107 | 77(91.7) | 0.005 |
| Yes | 2(5.1) | 4(6.6) | 9(12) | 9(12) | ||||
| Other | ||||||||
| No | 36(92.3) | 0.378 | 60(98.4) | 0.174 | 72(96) | 0.665 | 82(97.6) | 0.187 |
| Yes | 3(7.7) | 1(1.6) | 3(4) | 2(2.4) | ||||
| Does not ask anyone | ||||||||
| No | 32(82.1) | 0.423 | 51(83.6) | 0.512 | 62(82.7) | 0.299 | 69(82.1) | 0.193 |
| Yes | 7(17.9) | 10(16.4) | 13(17.3) | 15(17.9) | ||||
| ?² test,95% | ||||||||
| Failing scores in individual sections | ||||||||
| Source of SRH information | Female reproductive system n=39 (15.9%) | Male reproductive system n=61 (24.9%) | Knowledge of contraceptive methods n=75 (30.6%) | Failing scores for entire survey n=84 (34.3%) | ||||
| n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | |
| Mother | ||||||||
| No | 16(41) | 0.584 | 19(31.1) | 0.263 | 31(41.3) | 0.367 | 30(35.7) | 0.738 |
| Yes | 23(59) | 42(68.9) | 44(58.7) | 54(64.3) | ||||
| Father | ||||||||
| No | 24(61.5) | 0.093 | 39(63.9) | 0.082 | 55(73.3) | 0.853 | 54(64.3) | 0.036 |
| Yes | 15(38.5) | 22(36.1) | 20(26.7) | 30(35.7) | ||||
| Teacher | ||||||||
| No | 35(89.7) | 0.123 | 54(88.5) | 0.078 | 67(89.3) | 0.025 | 76(90.5) | 0.006 |
| Yes | 4(10.3) | 7(11.5) | 8(10.7) | 8(9.5) | ||||
| The Internet | ||||||||||
| No | 102(82.9) 0.717 | 94(86.2) 0.125 | 130(81. 8) | 0.877 | 55(91.7) 0.025 | 48(96) | 0.004 | |||
| Yes | 21(17.1) | 15(13.8) | 29(18.2) | 5(8.3) | 2(4) | |||||
| Other | ||||||||||
| No | 113(91.9) 0.019 | 106(97. 2) | 0.164 | 149(93. 7) | 0.170 | 56(93.3) 0.465 | 45(90) | 0.061 | ||
| Yes | 10(8.1) | 3(2.8) | 10(6.3) | 4(6.7) | 5(10) | |||||
| They do not ask anyone | ||||||||||
| No | 109(88.6) 0.257 | 90(82.6) 0.150 | 139(87. 4) | 0.424 | 50(83.3) 0.472 | 41(82) | 0.345 | |||
| Yes | 14(11.4) | 19(17.4) | 20(12.6) | 10(16.7) | 9(18) | |||||
| ?² test,95% | ||||||||||
| Source of SRH information: | Female reproductive system schematic diagram n=123 (50.2%) | Male reproductive system schematic diagram n=109 (44.5%) | Anatomical placement of contraceptive methods n=159 (64.9%) | Visual recognition of contraceptive methods n=60 (24.5%) | Schematic diagram of correct condom placement (9 steps) n=50 (20.4%) | |||||
| n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | |
| Mother | ||||||||||
| No | 45(36.6) 0.856 | 41(37.6) 0.891 | 59(37.1) | 0.987 | 25(41.7) 0.404 | 27(54) | 0.006 | |||
| Yes | 78(63.4) | 68(62.4) | 100(62. 9) | 35(58.3) | 23(46) | |||||
| Father | ||||||||||
| No | 81(65.9) 0.018 | 70(64.2) 0.009 | 112(70. 4) | 0.315 | 39(65) | 0.132 | 37(74) | 0.795 | ||
| Yes | 42(34.1) | 39(35.8) | 47(29.6) | 21(35) | 13(26) | |||||
| Teacher | ||||||||||
| No | 99(80.5) 0.896 | 91(83.5) 0.342 | 129(81. 1) | 0.864 | 51(85) | 0.344 | 42(84) | 0.522 | ||
| Yes | 24(19.5) | 18(16.5) | 30(18.9) | 9(15) | 8(16) | |||||
| Friends | ||||||||||
| No | 112(91.1) 0.811 | 101(92. 7) | 0.325 | 145(91. 2) | 0.671 | 55(91.7) 0.747 | 44(88) | 0.478 | ||
| Yes | 11(8.9) | 8(7.3) | 14(8.8) | 5(8.3) | 6(12) | |||||
| Health care center | ||||||||||
| No | 105(85.4) 0.837 | 92(84.4) 0.847 | 140(88. 1) | 0.061 | 54(90) | 0.204 | 44(88) | 0.492 | ||
| Yes | 18(14.6) | 17(15.6) | 19(11.9) | 6(10) | 6(12) | |||||
| Boyfriend/girlfriend | ||||||||||
| No | 121(98.4) 0.993 | 108(99. 1) | 0.429 | 156(98. 1) | 0.670 | 57(95) | 0.018 | 49(98) | 0.818 | |
| Yes | 2(1.6) | 1(0.9) | 3(1.9) | 3(5) | 1(2) | |||||
| Year 2 020 | |||||||||
| Failing scores in individual sections | Failing scores for entire survey | ||||||||
| G ) Volume XX Issue VI Version I | Source of SRH information: Mother No Yes Father No Yes | Female reproductive system OR CI 95% 1 0.82 (0.41 -1.65) 1 1.84* (0.90 -3.77) | Male reproductive system OR CI 95% 1 1.42 (0.77 -2.64) 1 1.73* (0.93 -3.22) | Knowledge of contraceptive methods OR CI 95% 1 0.77 (0.44 -1.35) 1 0.94 1.74) (0.51 - | Failing scores for entire survey OR CI 95% 1 1.10 (0.63 -1.90) 1 1.85** (1.04 -3.29) | ||||
| ( | Teacher | ||||||||
| Global Journal of Computer Science and Technology | No Yes Friends No Yes Health care center No Yes Boyfriend/girlfriend No Yes The Internet No Yes Other No Yes Does not ask anyone | 1 0.43 1 0.78 1 1.58 --1 0.21** 1 1.82 | (0.15 -1.29) (0.22 -2.75) (0.66 -3.76) --(0.05 -0.91) (0.47 -7.06) | 1 0.47* 1 0.26* 1 0.81 --1 0.25** 1 0.26 | (0.20 -1.10) (0.06 -1.16) (0.35 -1.87) --(0.09 -0.74) (0.03 -2.07) | 1 0.40** 1 0.60 1 0.39** --1 0.53 1 0.75 | (0.18 -0.91) (0.22 -1.69) (0.16 -0.98) --(0.24 -1.16) (0.20 -2.83) | 0.33*** 1 0.50 1 0.67 1 0.63 1 0.30*** 1 0.37 | (0.15 -0.74) (0.18 -1.41) (0.31 -1.46) (0.06 -6.20) (0.13 -0.72) (0.08 -1.72) |
| No | 1 | 1 | 1 | 1 | |||||
| Yes | 1.45 | (0.58 -3.61) | 1.31 | (0.59 -2.92) | 1.49 | (0.70 -3.16) | 1.62 | (0.78 -3.39) | |
| *** p<0.01, ** p<0.05, * p<0.1 | |||||||||
| Failing scores in individual diagrams | ||||||||||
| Source of SRH information | Female reproductive system schematic diagram | Male reproductive system schematic diagram | Anatomical placement of contraceptive method | Visual recognition of CM | Schematic diagram of correct condom placement (9 steps) | |||||
| OR | CI 95% | OR | CI 95% | OR | CI 95% | OR | CI 95% | OR | CI 95% | |
| Mother | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 1.05 (0.62 -1.76) | 0.96 | (0.57 -1.62) | 1.00 (0.58 -1.73) | 0.78 | (0.43 -1.41) | 0.42** * | (0.22 -0.78) | ||
| Father | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 1.99 ** | (1.12 -3.54) | 2.13** * | (1.20 -3.77) | 1.36 (0.74 -2.50) | 1.62 | (0.86 -3.02) | 0.91 | (0.45 -1.84) | |
| Teacher | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 1.04 (0.55 -1.97) | 0.73 | (0.38 -1.40) | 0.94 (0.49 -1.83) | 0.68 | (0.31 -1.51) | 0.76 | (0.33 -1.75) | ||
| Friends | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 0.90 (0.38 -2.13) | 0.64 | (0.26 -1.57) | 0.83 (0.34 -2.00) | 0.84 | (0.30 -2.38) | 1.43 | (0.53 -3.83) | ||
| Health care | ||||||||||
| center | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 0.93 (0.46 -1.87) | 1.07 | (0.53 -2.16) | 0.51 * | (0.25 -1.04) | 0.55 | (0.22 -1.40) | 0.72 | (0.28 -1.84) | |
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 0.99 (0.14 -7.16) | 0.41 | (0.04 -4.00) | 1.63 | (0.17 -15.96) | 9.68* | (0.99 -94.92) | 1.31 | (0.13 -12.83) | |
| The Internet | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 0.89 (0.46 -1.70) | 0.59 | (0.30 -1.16) | 1.06 (0.53 -2.10) | 0.34** | (0.13 -0.91) | 0.15** | (0.04 -0.65) | ||
| Other | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 5.31 ** | (1.14 -24.76) | 0.40 | (0.11 -1.51) | 2.82 | (0.60 -13.17) | 1.58 | (0.46 -5.45) | 2.98* | (0.91 -9.84) |
| Does do not | ||||||||||
| ask anyone | ||||||||||
| No | 1 | 1 | 1 | 1 | 1 | |||||
| Yes | 0.66 (0.31 -1.37) | 1.70 | (0.82 -3.53) | 0.74 (0.35 -1.55) | 1.34 | (0.60 -3.00) | 1.49 | (0.65 -3.44) | ||
| *** p<0.01, ** p<0.05, * p<0.1 | ||||||||||
| 9th | 47(30.5) | 17(25.4) | 26(55.3) | 12(52.2) | |||||
| Belongs to indigenous group (self-report) | |||||||||
| Yes | 129(88.4) 0.631 | 61(93.8) | 0.068 | 43(91.5) | 0.360 | 19(86.4) | 0.859 | ||
| No | 17(11.6) | 4(6.2) | 4(8.5) | 3(13.6) | |||||
| Family structure (lives with) | |||||||||
| Both parents | 110(71.4) 0.688 | 61(91) | 0.000 | 28(59.6) | 0.173 | 10(43.5) | 0.011 | ||
| Mother | 39(25.3) | 5(7.5) | 16(34) | 11(47.8) | |||||
| Father, grandfather, uncle | 5(3.2) | 1(1.5) | 3(6.4) | 2(8.7) | |||||
| Mother's level of schooling | |||||||||
| Up to high school | 69(50.4) | 0.241 | 26(44.8) | 0.781 | 20(51.3) | 0.461 | 12(54.5) | 0.812 | |
| High school | 41(29.9) | 17(29.3) | 8(20.5) | 5(22.7) | |||||
| High school+ | 27(19.7) | 15(25.9) | 11(28.2) | 5(22.7) | |||||
| Father's level of schooling | |||||||||
| Up to high school | 61(54.5) | 0.533 | 21(40.4) | 0.097 | 16(50) | 0.914 | 13(81.3) | 0.049 | |
| High school | 29(25.9) | 17(32.7) | 8(25) | 1(6.3) | |||||
| High school+ | 22(19.6) | 14(26.9) | 8(25) | 2(12.5) | |||||
| Mother's age range (yrs) | |||||||||
| <30 | 19(12.7) | 0.510 | 8(12.5) | 0.623 | 1(2.2) | 0.024 | 2(9.1) | 0.273 | |
| 30 -40 | 77(51.3) | 37(57.8) | 23(50) | 9(40.9) | |||||
| 40+ | 54(36) | 19(29.7) | 22(47.8) | 11(50) | |||||
| Father's age range (yrs) | |||||||||
| <30 | 6(4.3) | 0.658 | 2(3.1) | 0.224 | 1(2.4) | 0.233 | 1(5.6) | 0.881 | |
| Boyfriend/ | 30 -40 | 56(40.6) | 33(51.6) | 13(31.7) | 7(38.9) | ||||
| girlfriend | 40+ | 76(55.1) | 29(45.3) | 27(65.9) | 10(55.6) | ||||
| Source of SRH information* | |||||||||
| Mother | Father | Teacher | Friends | ||||||
| n= 154(62.9%) | n=67 (27.5%) | n=47 (19.2%) | n=23 (9.4%) | ||||||
| n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | ||
| Gender | |||||||||
| Women | 93(60.4) | 0.000 | 24(35.8) | 0.003 | 24(51.1) | 0.956 | 12(52.2) | 0.940 | |
| Men | 61(39.6) | 43(64.2) | 23(48.9) | 11(47.8) | |||||
| School year currently enrolled in (grade) | |||||||||
| 7th | 61(39.6) | 0.042 | 22(32.8) | 0.036 | 6(12.8) | 0.001 | 3(13) | 0.064 | |
| 8th | 46(29.9) | 28(41.8) | 15(31.9) | 8(34.8) | |||||
| Both parents | 27(73) | 0.796 | 4(100) | 0.796 | 27(61.4) 0.315 | 6(50) | 0.050 | 25(73.5) | 0.895 | |
| Mother | 8(21.6) | 0(0) | 15(34.1) | 4(33.3) | 8(23.5) | |||||
| Father, grandfather, uncle | 2(5.4) | 0(0) | 2(4.5) | 2(16.7) | 1(2.9) | |||||
| Mother's level of | ||||||||||
| schooling | ||||||||||
| Up to high school 12(41.4) | 0.218 | 1(33.3) | 0.218 | 20(50) | 0.148 | 7(58.3) | 0.657 | 12(48) | 0.865 | |
| High school | 12(41.4) | 0(0) | 7(17.5) | 2(16.7) | 8(32) | |||||
| High school+ | 5(17.2) | 2(66.7) | 13(32.5) | 3(25) | 5(20) | |||||
| Father's level of | ||||||||||
| schooling | ||||||||||
| Up to high school 11(47.8) | 0.272 | 1(33.3) | 0.272 | 17(53.1) 0.506 | 5(55.6) | 0.670 | 12(60) | 0.768 | ||
| High school | 4(17.4) | 2(66.7) | 10(31.3) | 3(33.3) | 4(20) | |||||
| High school+ | 8(34.8) | 0(0) | 5(15.6) | 1(11.1) | 4(20) | |||||
| Mother's age | ||||||||||
| range (yrs) | ||||||||||
| <30 | 1(2.9) | 0.212 | 1(25) | 0.212 | 4(9.5) | 0.905 | 0(0) | 0.044 | 3(9.7) | 0.878 |
| 30 -40 | 20(57.1) | 1(25) | 23(54.8) | 4(33.3) | 18(58.1) | |||||
| 40+ | 14(40) | 2(50) | 15(35.7) | 8(66.7) | 10(32.3) | |||||
| Father's age range | ||||||||||
| (yrs) | ||||||||||
| <30 | 0(0) | 0.034 | 1(25) | 0.034 | 1(2.8) | 0.940 | 0(0) | 0.530 | 0(0) | 0.455 |
| 30 -40 | 9(26.5) | 0(0) | 15(41.7) | 3(30) | 13(50) | |||||
| 40+ | 25(73.5) | 3(75) | 20(55.6) | 7(70) | 13(50) | |||||
| Source of SRH information* | ||||||||||
| Health center n=37 (15.1%) | Boyfriend/girlfriend n=4 (1.6%) | The Internet n= 44(17.9%) | Other n= 12(4.9%) | Does not ask anyone n=34 (13.9%) | ||||||
| n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | |
| Gender | ||||||||||
| Women | 14(37.8) | 0.073 | 3(75) | 0.073 | 23(52.3) 0.902 | 6(50) | 0.919 | 16(47.1) | 0.583 | |
| Men | 23(62.2) | 1(25) | 21(47.7) | 6(50) | 18(52.9) | |||||
| School year | ||||||||||
| currently enrolled | ||||||||||
| in (grade) | ||||||||||
| 7th | 11(29.7) | 0.565 | 1(25) | 0.565 | 6(13.6) | 0.000 | 2(16.7) | 0.381 | 12(35.3) | 0.360 |
| 8th | 10(27) | 1(25) | 11(25) | 4(33.3) | 7(20.6) | |||||
| 9th | 16(43.2) | 2(50) | 27(61.4) | 6(50) | 15(44.1) | |||||
| Belongs to | ||||||||||
| indigenous group | ||||||||||
| (self-report) | ||||||||||
| No | 28(77.8) | 0.053 | 3(75) | 0.053 | 38(88.4) 0.857 | 9(75) | 0.176 | 28(87.5) | 0.992 | |
| Yes | 8(22.2) | 1(25) | 5(11.6) | 3(25) | 4(12.5) | |||||
| Family structure | ||||||||||
| (lives with) | ||||||||||